 There are more than 100 different forms of cleft
There are more than 100 different forms of cleft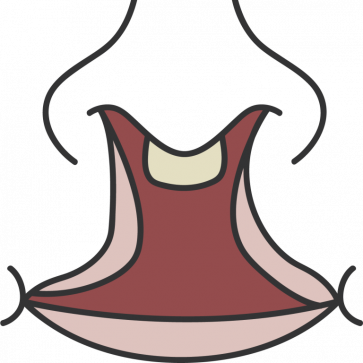
 There are more than 100 different forms of cleft
There are more than 100 different forms of cleft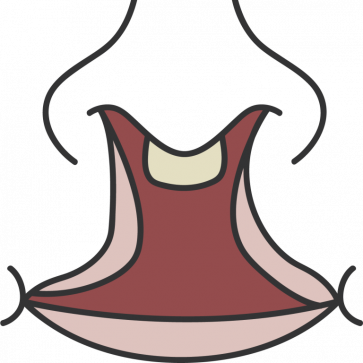
Cleft knowledge
Everything you need to know about cleft lip and palate
1. What is cleft?
Cleft, short for cleft lip and palate, is one of the most common birth defects in the world. The name of our organization, “Deutsche Cleft Kinderhilfe”, translates to German Cleft Children’s Aid Society.
Children with cleft lip and palate are born on every continent in the world. Worldwide, it is thought that on average one of every 500 to 600 children born is born with cleft. Certain risk factors make cleft more likely in some regions than in others. For example the likelihood of a child having cleft is thought to be slightly higher in Asia and slightly lower in Africa.
“Harelip” or cleft?
The cleft lip was long colloquially known as the harelip. In German, the cleft palate was also known as a “Wolfsrachen”, a wolf’s maw. This sort of animal imagery is perceived as degrading by many patients with cleft lip and palate. These terms should therefore no longer be used to describe cleft lip and palate.
The term harelip can be found in old medical books from the 15th century. The association was not limited to the superficial visual resemblance of some clefts to a to a hare’s upper lip. There also was the superstition that cleft lip was caused by a pregnant woman having looked at or thought of a hare. Fortunately, this superstition was eventually overcome, but even in 1805 a doctor was forced to point out that if the superstition were true, the wives of hunters and butchers should have nothing but children with cleft, which was demonstrably false.
The term harelip however lasted much longer in colloquial and even medical usage and unfortunately is sometimes still used today. It should be avoided in favor of the correct terms “cleft lip” and / or “cleft palate”. You can read more about this topic in our article.
 "cleft palate"
"cleft palate" "cleft lip"
"cleft lip" The term “harelip” is considered demeaning by many people with cleft.
The term “harelip” is considered demeaning by many people with cleft.2. Causes of cleft lip and palate
The baby’s face is formed between the fifth and eleventh week of pregnancy. During this time, the lips develop, as well as the front section of the jaw and the hard and soft palate. If the process is interfered with by one or more of the risk factors, a cleft can result.
The exact causes of a case of cleft lip and / or palate cannot be clearly identified. A cleft usually is the result of a combination of factors. This is called a multifactorial origin.
We know that a higher risk of cleft can be inherited from the child’s parents. Other, outside risk factors can further add to the risk before and during pregnancy. These can be for example pollution of the environment and food, unfavorable habits (alcohol, nicotine, other drugs), malnutrition and diseases of the mother which are often a problem in poor families, lack of oxygen at high altitudes and other effects.
 A cleft is more likely, but not certain, if one or both parents have cleft themselves.
A cleft is more likely, but not certain, if one or both parents have cleft themselves.Can the development of a cleft lip and palate be prevented?
As we have seen, a case of cleft lip and palate does not have one clear cause. Accordingly, there is no way to completely prevent them. The risk of cleft can at best be lowered, for example through measures such as vitamin supplements (for example folate, also known as vitamin B9), and a generally health-conscious lifestyle during pregnancy.
Unlike in the West, where prenatal care and maternity protection are mandated by law, women in our project countries can’t avoid many of the risk factors during pregnancy. They may not have enough food, or the food they can get may lack important nutrients. Many are exposed to pollution and environmental poisons. The expectant mothers rarely have access to medical care and are often forced to work hard until the birth under conditions that are harmful to health.
3. Types of cleft
What kinds of cleft are there?
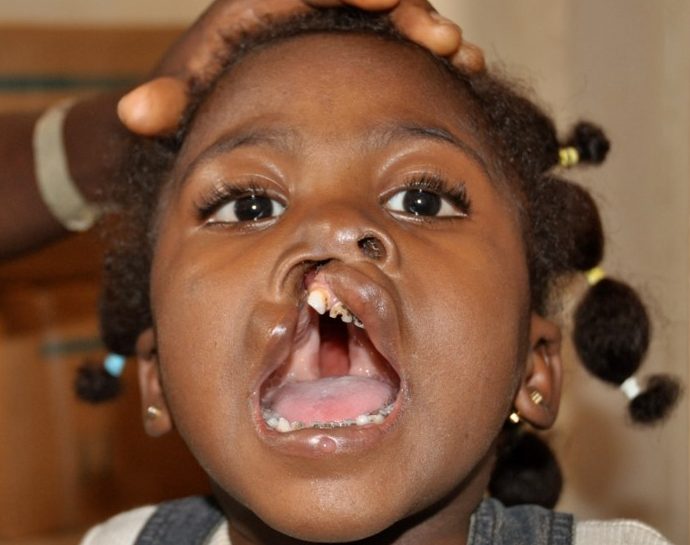
There are more than 100 different forms of cleft, which in everyday language are all combined under the umbrella term cleft lip and palate. The differences between the types concern the location, severity, and the appearance of the cleft.
Cleft locations
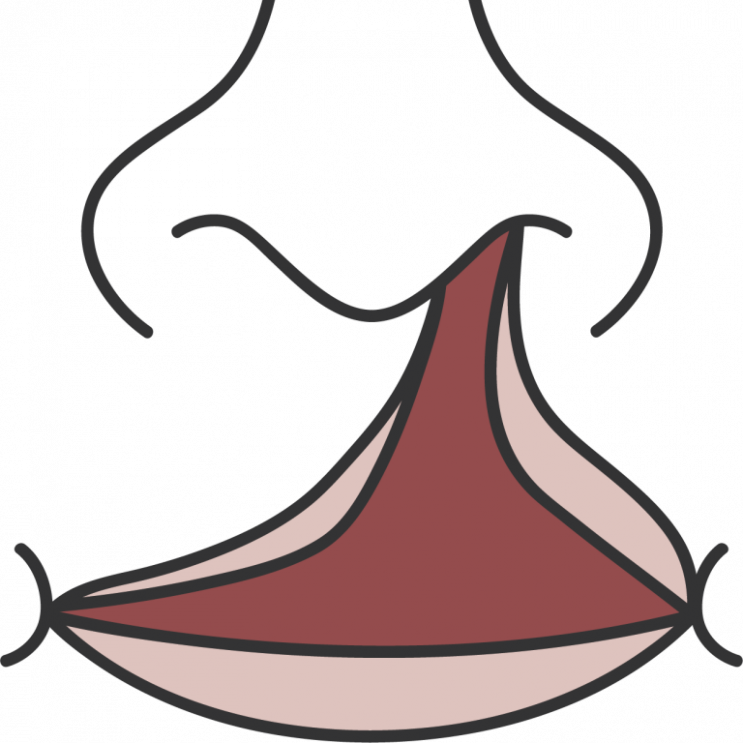
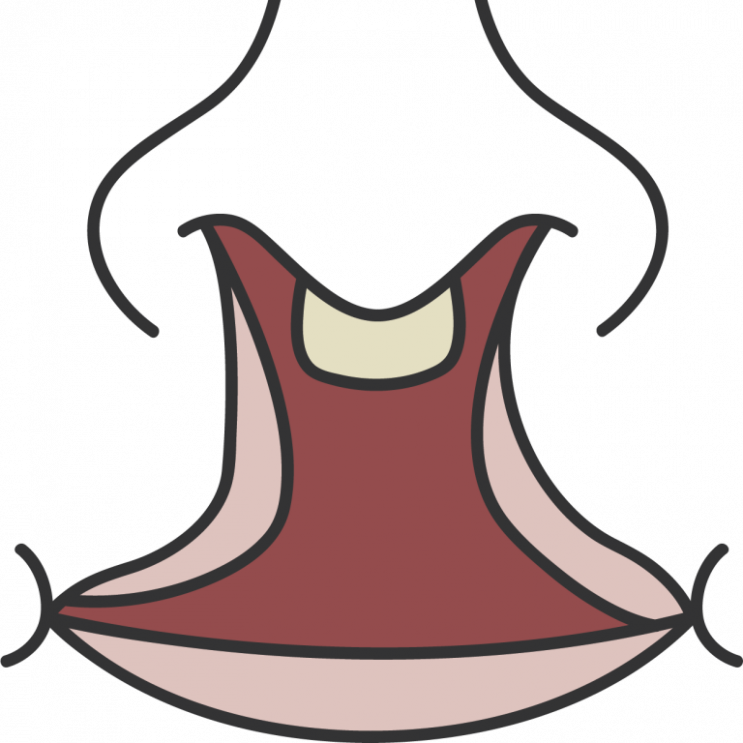
Cleft most often occurs in four places: Cleft lip, or cleft lip and upper jaw, or cleft lip and palate usually develop at the end of the second month of pregnancy and affect more boys than girls.
Isolated clefts in the hard and soft palate develop early in the third month of pregnancy. They are less common, and occur a little more often in girls than in boys. The cleft can affect the hard and soft palate or be limited to the soft palate.
See the picture below for the locations. The picture shows the roof of the mouth looking up from below, with the nose at the very top of the picture.
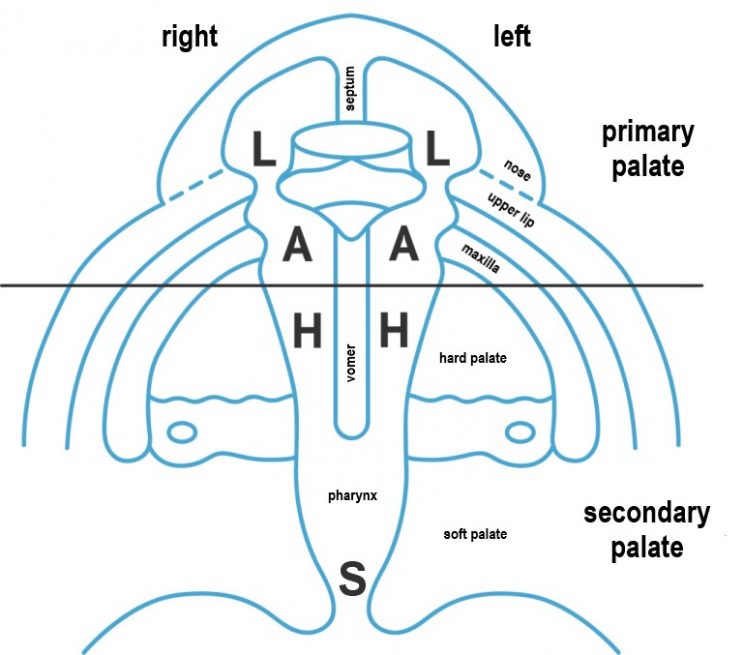
L: Lip
Upper lip including the nostril
A: Jaw
Tooth-bearing part of the upper jaw (alveolar process)
H: Hard Palate
Palate roof with nasal floor (bony part of the palate)
S: Soft Palate
Soft palate (muscular part of the palate)
Severity of a cleft
There are three levels of severity of a cleft lip and palate:
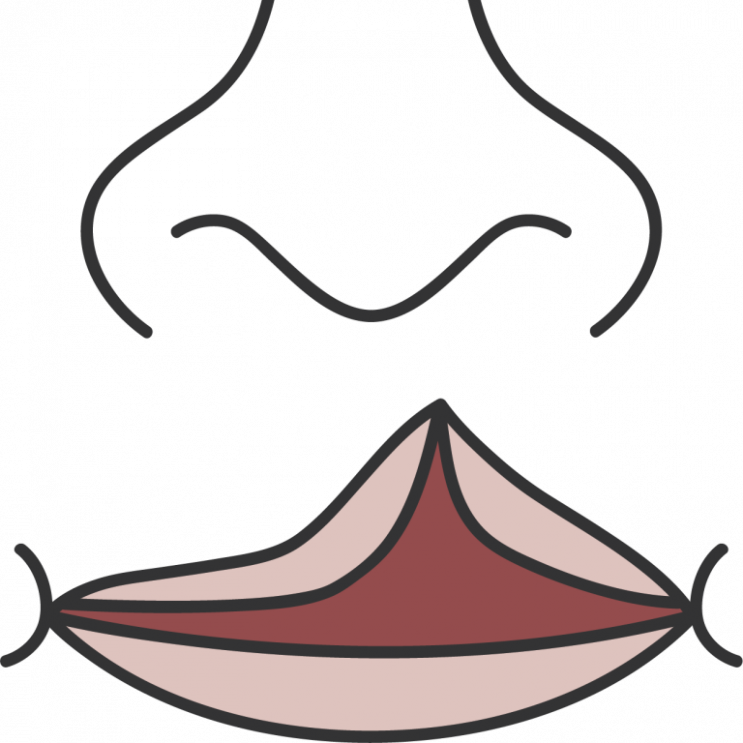
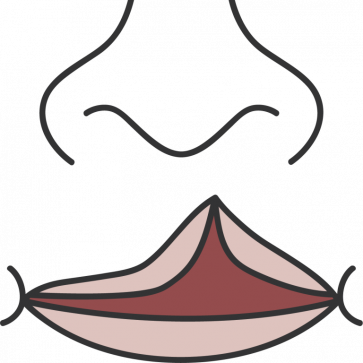
Partial cleft (microform)
Only the upper lip is affected by the cleft. The cleft does not extend to the nostril.
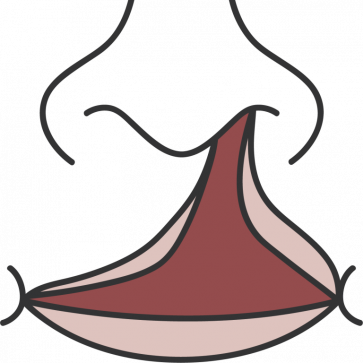
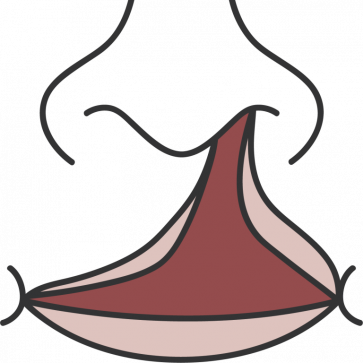
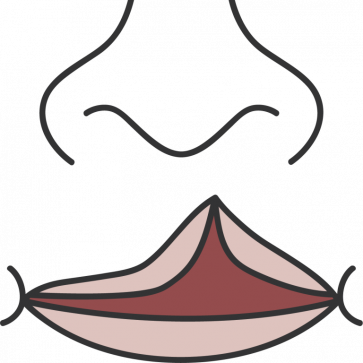
Complete cleft, unilateral
Cleft of the muscle and/or bone including the covering skin and mucosa, on one side of the lip.
Complete cleft, bilateral
Cleft of the muscle and/or bone including the covering skin and mucosa, on both sides of the lip.
All clefts, with the exception of that of the soft palate, can occur on the left, the right, or on both sides at once. The extent of the cleft is often not directly visible in the partial clefts. Even if the soft palate is closed with mucous membrane, leaving no visible cleft, the cleft of the muscles underneath the mucous membrane results in problems speaking and/or a ventilation disorder of the middle ear.
Cleft lip and palate, unilateral

Cleft palate

Complete cleft, unilateral

Complete cleft, bilateral

Partial cleft, (microform)
4. Consequences of a cleft lip and palate
More than just an aesthetic problem
A cleft is a highly visible “flaw”. Depending on its size and severity the children are disfigured more or less. Because they are perceived as different, the children are often teased or shunned. Often they live their lives in isolation. The psychological and emotional stress for child and parents is enormous. Children who have no access to treatment or are treated late in life suffer more.
Functional consequences: Swallowing, breathing, speaking
If the palate is affected there is no separation of the mouth and nasal cavity. This means that the muscles of the lips, tongue and palate do not work together properly, and there is often a change in the position of the tongue, which moves backwards into the cleft. Serious functional problems are the result: swallowing and breathing, sound formation and tone of voice are affected.
In babies the breathing and feeding problems can be deadly: the children are often undernourished, which leaves them vulnerable to infectious diseases. Later in life, food leaking out through the nose can continue to be a problem and a source of shame for patients if the cleft is not treated. The difficulty in forming certain sounds means that speech development is impaired. Hearing deficits due to chronic middle ear infections worsen these problems. The children are often stigmatized because of their difficult to understand pronunciation and often nasal voice.
Together with the formation of scars due to the surgeries, these functional disorders can also lead to impairments in the position of the teeth and the development of the jaw and face later in life as the child grows, requiring ongoing monitoring and care.
5. Treatment of cleft lip and palate: How is cleft lip and palate treated?
The foundation of the treatment: the surgery
The surgery is the first and most important step for a child with cleft lip and palate. The lip is usually closed in the first three months of life. A cleft palate is closed between the eighth and eleventh month. More surgeries are often necessary later.
Thanks to our healthcare systems, the costs for the necessary treatments are covered by the health insurance in developed countries. This however is not the case all over the world. In many countries, parents have to pay for their child’s treatment themselves. But many families cannot raise the money. Without treatment, the children suffer from the mental and physical consequences of the malformation for their entire lives.
Interdisciplinary cleft care
Due to the many different health problems the patients have, many medical specialists have to work together closely in many therapy steps taken in the right order to repair the damage and get the best outcome for the child. The medical specialties involved include orthodontics, maxillofacial surgery, pediatrics, ear, nose and throat medicine / pediatric audiology, speech therapy / phoniatrics, psychology, pediatric dentistry and nutrition. Depending on the severity of the cleft, therapy can stretch into adulthood. For all types of cleft, regular routine check-ups are recommended until development is complete (19 to 21 years).
Overview of issues and therapies:
Störungen und Behandlungsmöglichkeiten im Überblick
Aussehen, Mimik → Operation Lippe, NAM-Therapie (präoperativ)
Schlucken, Atmen → Operation Gaumen
Mittelohrbelüftung / Hörminderung → HNO-Betreuung, funktionelle Sprachtherapie
Sprache / Stimmklang → Funktionelle Sprachtherapie, operative Verfahren
Zahnfehlstellung / Zahngesundheit → Zahnärztliche Betreuung
Kiefer- und Gesichtsschädel-entwicklung → Kieferorthopädische / kieferchirurgische Behandlung
appearance, facial expressions
swallowing, breathing
middle ear ventilation / hearing impairment
speech / phonetics
misalignment of teeth / dental health
development of the jaw and facial bones
→
→
→
→
→
→
lip surgery, NAM therapy (preoperative)
palate surgery
ENT care, functional speech therapy
functional speech therapy, surgical therapies
dental / orthodontic care
orthodontic / maxillofacial surgery care

Surgery
The surgery to close the cleft is the first and central therapeutic measure. It represents a decisive turning point in the life of a child with cleft lip and palate.

Speech- and Functional Therapy
Cleft children are impaired in their speech development due to dysfunction in the structures of the mouth, jaw and throat. The oral muscles are underdeveloped and children with a cleft palate also have a nasal, often hoarse speech. Oral motor skills and articulation are improved through speech and functional therapy.

Dentistry / Orthodontics
A cleft lip and palate is often accompanied by severe misalignments of the teeth and jaw. Correcting these is a long-term process. It is not uncommon for subsequent surgical interventions, such as bone transplants, to be necessary. In some of our treatment centers, children are treated with NAM therapy before surgery. In addition, almost all children in our project countries have bad teeth due to a lack of dental care and oral hygiene.

ENT Care
As a result of a cleft palate, there is insufficient pressure equalization in the middle ear. This restricts the ventilation of the middle ear, resulting in fluid build-up. The children suffer from a constant feeling of pressure, earache and, in many cases, chronic middle ear infections. In the long term, the build-up of fluid in the middle ear leads to hearing damage and subsequently problems in learning to speak.
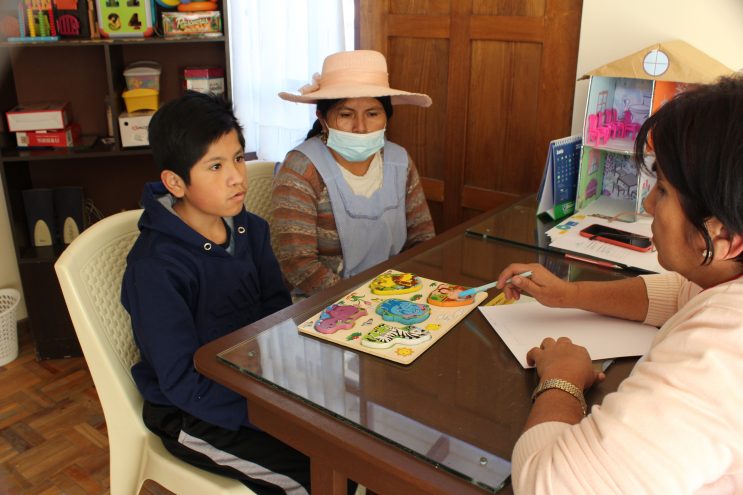
Psychosocial Support
Cleft children are different from other children. They look different, talk differently. Being different often leads to exclusion, ridicule and mobbing. This can result in far-reaching psychosocial disorders for the children. Early and continuous psychological support helps to promote the children's self-confidence. It also helps the affected parents, for whom the birth of a child with a cleft is a great burden.
6. Support for cleft patients
Support in Germany
Exchange of experiences with other affected families can relieve stress and provide new insights. Suitable contacts can be made via the nationwide self-help association for lip and palate malformations of the Wolfgang Rosenthal Society and the IFUS e.V. society for the aid and support for cleft patients with contact points in Saxony, Saxony-Anhalt and Thuringia.
Caring for a child with cleft lip and palate is particularly demanding in the first few years and can also carry considerable financial cost. To address this, the federal government has created the so-called “degree of disability” („Grad der Behinderung“, GdB). Depending on the type of cleft, various degrees of disability can be applied for as the basis for financial aid. Depending on the care expenditure, a care allowance can be applied for.
Further information is provided by the German interdisciplinary working group for cleft lip and palate / craniofacial anomalies (AK-LKG). We thank the AK-LKG for giving us permission to use the pictorical material used on this page.
Support in developing countries
In Germany, the costs for all necessary treatments are covered by the universal healthcare providers. Children in developing countries often have no access to qualified treatment, and their parents receive no support. Proper treatment is out of their financial reach, medical infrastructure and qualified surgeons are often not available. In these countries, NGOs like Deutsche Cleft Kinderhilfe provide the necessary treatment to these children – as a prerequisite for a dignified, healthy life.

